

Psychosocial Aspects of Fertility and Assisted Reproductive Technology – Dr. Jamie Stanhiser
Psychosocial aspects of fertility, infertility, and assisted reproductive technology (ART) can significantly impact patients’ sense of self-identity and personal agency, mental well-being, sexual and marital relationships, reproductive efficiency, compliance with treatment, and pregnancy outcomes. Research is needed to understand how stress, anxiety, depression, mood disorders, and psychotropic medications impact fertility and infertility treatment. The psychosocial implications of ART on our society include a shift toward older maternal age at conception, the complexities of third-party reproduction, and consideration for the psychological and socioeconomic barriers to receiving care. Clinicians must understand, screen for, and identify couples struggling with the psychological and social aspects of fertility and ART.
Stanhiser J, Steiner A. Psychosocial Aspects of Fertility and Assisted Reproductive Technology. Obstet Gynecol Clin North Am. 2018 Sep;45(3:563-574. PMID: 30092929
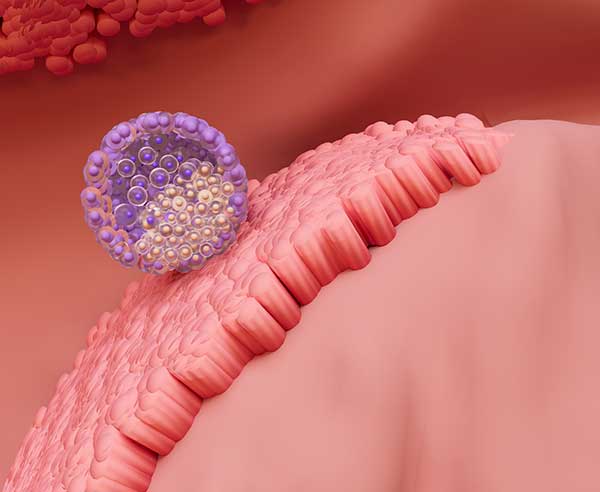

First Case Report of a Healthy Live Birth Following a Frozen Embryo Transfer of a Day 8 Euploid Blastocyst – Dr. Jamie Stanhiser & Dr. Gabriel Garzo
Objective: To report a case of a healthy live birth following a frozen embryo transfer of a euploid blastocyst after 8 days of culture.
Materials and Methods: Case report of a 40-year-old G6P1051 female who presented to a fertility center with recurrent pregnancy loss of unknown etiology, as well as male factor and age-related infertility. She underwent two sequential IVF cycles with pre-implantation genetic testing for aneuploidy (PGT-A) by Next Generation Sequencing, with a subsequent frozen embryo transfer (FET) using a gestational carrier two years later.
Results: Three blastocyst embryos were produced: Day 5 (5AA) aneuploid male; a Day 7 (5BC) euploid female; and a Day 8 (6AB) euploid male. Due to the perceived low implantation potential of a Day 8 blastocyst, a double embryo transfer of the Day 7 female and the Day 8 male euploid embryos was performed in a FET cycle using a gestational carrier. The double embryo transfer resulted in a singleton pregnancy and the birth of a normal health baby male weighing 4,252 g after 39 weeks’ gestation.
Conclusions: Although their development is delayed, euploid blastocysts with good morphological grade after 8 days of culture can be viable, and can result in a healthy live birth.
Impact Statement: To our knowledge, this is the first case report of a live birth after the transfer of an euploid embryo after 8 days of culture. Although a rare occurrence, good quality embryos after 8 days of culture should be considered for embryo transfer. Because of the high risk of aneuploidy, PGT-A should be performed.
Stanhiser J, Yeo AL, Fuller AD, Garzo VG. First Case Report of a Healthy Live Birth Following a Frozen Embryo Transfer of A Day 8 Euploid Blastocyst. Fertil Steril. 2021 Sep; 116(3):E279.


Endometriosis is a chronic systemic disease: clinical challenges and novel innovations – Dr. Valerie Flores
Endometriosis is a common disease affecting 5-10% of women of reproductive age globally. However, despite its prevalence, diagnosis is typically delayed by years, misdiagnosis is common, and delivery of effective therapy is prolonged. Identification and prompt treatment of endometriosis are essential and facilitated by accurate clinical diagnosis. Endometriosis is classically defined as a chronic, gynaecological disease characterised by endometrial-like tissue present outside of the uterus and is thought to arise by retrograde menstruation. However, this description is outdated and no longer reflects the true scope and manifestations of the disease. The clinical presentation is varied, the presence of pelvic lesions is heterogeneous, and the manifestations of the disease outside of the female reproductive tract remain poorly understood. Endometriosis is now considered a systemic disease rather than a disease predominantly affecting the pelvis. Endometriosis affects metabolism in liver and adipose tissue, leads to systemic inflammation, and alters gene expression in the brain that causes pain sensitisation and mood disorders. The full effect of the disease is not fully recognised and goes far beyond the pelvis. Recognition of the full scope of the disease will facilitate clinical diagnosis and allow for more comprehensive treatment than currently available. Progestins and low-dose oral contraceptives are unsuccessful in a third of symptomatic women globally, probably as a result of progesterone resistance. Oral gonadotropin-releasing hormone (GnRH) antagonists constitute an effective and tolerable therapeutic alternative when first-line medications do not work. The development of GnRH antagonists has resulted in oral drugs that have fewer side-effects than other therapies and has allowed for rapid movement between treatments to optimise and personalise endometriosis care. In this Review, we discuss the latest understanding of endometriosis as a systemic disease with multiple manifestations outside the parameters of classic gynecological disease.
Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. Lancet. 2021 Feb 27; 397 (10276): 839-852. PMID: 33640070.


Omega-3 fatty acid supplementation and fecundability – Dr. Jamie Stanhiser
Study question: Is self-reported use of omega-3 fatty acid supplements associated with fecundability, the probability of natural conception, in a given menstrual cycle?
Summary answer: Prospectively recorded omega-3 supplement use was associated with an increased probability of conceiving.
What is known already: In infertile women, omega-3 fatty acid intake has been associated with increased probability of pregnancy following IVF. In natural fertility, studies are conflicting, and no study of natural fertility has evaluated omega-3 fatty acid supplementation and fecundity.
Study design, size, duration: Secondary data analysis of 900 women contributing 2510 cycles in Time to Conceive (TTC), a prospective, time to pregnancy cohort study from 2008 to December 2015.
Participants/materials, setting, methods: Women aged 30-44 years, trying to conceive <3 months, without history of infertility were followed using standardized pregnancy testing. While attempting to conceive, women daily recorded menstrual cycle events and supplement and medication intake using the Cerner Multum Drug Database. Supplements and vitamins containing omega-3 were identified. Omega-3 use, defined as use in at least 20% of days in a given menstrual cycle, in each pregnancy attempt cycle was determined. A discrete-time Cox proportional hazards model was used to calculate the fecundability ratio.
Main results and the role of chance: Women taking omega-3 supplementation were more likely to be younger, thinner, nulligravid, white and to take vitamin D, prenatal and multivitamins compared to women not taking omega-3s. After adjusting for age, obesity, race, previous pregnancy, vitamin D and prenatal and multivitamin use, women taking omega-3 supplements had 1.51 (95% CI 1.12, 2.04) times the probability of conceiving compared to women not taking omega-3s.
Limitations, reasons for caution: Our study was not a randomized controlled trial. The women who used omega-3 supplements may represent a more health-conscious population. We sought to address this by adjusting for multiple factors in our model. Additionally, the omega-3 fatty acid supplements that TTC participants used included multiple types and brands with varying dosages of omega-3 fatty acids. Women reported the type of supplement they were taking but not the concentration of omega-3s in that supplement. It is therefore not possible to compare dosing or a dose-response relationship in our study.
Wider implications of the findings: Omega-3 supplementation may present a feasible and inexpensive modifiable factor to improve fertility. Randomized controlled trials are needed to further investigate the benefits of omega-3 supplementation for women trying to conceive naturally.
Stanhiser J, Jukic AMZ, McConnaughey DR, Steiner AZ. Omega-3 fatty acid supplementation and fecundability. Hum Reprod. 2022 May 3;37(5):1037-1046. PMID: 35147198


Pre-IVF treatment with a GnRH antagonist in women with endometriosis (PREGNANT): study protocol for a prospective, double-blind, placebo-controlled trial – Dr. Valerie Flores
Introduction: Infertility is a common complication of endometriosis. While in vitro fertilisation-embryo transfer (IVF) successfully treats endometriosis-associated infertility, there is some evidence that pregnancy rates may be diminished in women seeing fertility treatment for endometriosis-associated infertility compared with other etiologies of infertility. The use of gonadotropin releasing hormone (GnRH) agonist prior to IVF has been suggested to improve success, however studies have been small and rarely reported live birth rates. Recent approval of an oral GnRH antagonist for endometriosis provides a novel option for women with endometriosis who are undergoing IVF. There have been no studies on the efficacy of GnRH antagonists for the treatment of endometriosis-related infertility.
Methods and analysis: This study is a multicentre, prospective, randomised, double-blind, placebo-controlled trial to study the efficacy of GnRH antagonist pretreatment for women with endometriosis who are undergoing IVF. A total of 814 patients with endometriosis undergoing fertility treatment will be enrolled and randomised 1:1 into two groups: elagolix 200 mg two times per day or placebo for 8 weeks, prior to undergoing IVF. All participants will then undergo IVF treatment per local protocols. The primary outcome is live birth. Secondary outcomes include oocyte number, fertilisation rate, embryo morphology and implantation rates, as well as rates of known endometriosis-related obstetrical outcomes (pregnancy-induced hypertension, antepartum haemorrhage, caesarean delivery and preterm birth).
Ethics and dissemination: The PREGnant trial was approved by the Institutional Review Board at Johns Hopkins University. Results will be published in a peer-reviewed journal.
Trial registration number: NCT04173169.
Taylor H, Li HK, Carson S, Flores V, Pal L, Robbins J, Santoro NF, Segars JH, Seifer D, Huang H, Young S, Zhang H. Pre-IVF treatment with a GnRH antagonist in women with endometriosis (PREGNANT): study protocol for a prospective, double-blind, placebo-controlled trial. BMJ Open. 2022 Jun 17; 12(6):e052043.
PMID: 35715184.


Bazedoxifene-Conjugated Estrogens for Treating Endometriosis – Dr. Valerie Flores
Background: Endometriosis is a gynecologic disorder affecting 6-10% of reproductive-aged women. First-line therapies are progestin-based regimens; however, failure rates are high, often requiring alternative hormonal agents, each with unfavorable side effects. Bazedoxifene with conjugated estrogens is approved for treatment of menopausal symptoms, and use in animal studies has demonstrated regression of endometriotic lesions. As such, it represents a potential treatment option for endometriosis.
Case: A patient with stage III endometriosis referred for management of dysmenorrhea and cyclic pelvic pain was treated with 20 mg bazedoxifene and 0.45 mg conjugated estrogens daily for more than 6 months. She noted resolution of pelvic pain. There were no abnormal effects on hormonal, uterine, or ovarian parameters.
Conclusion: Bazedoxifene with conjugated estrogens may be an effective alternative to traditional endometriosis treatment options.
Flores VA, Stachenfeld NS, Taylor HS. Bazedoxifene-Conjugated Estrogens for Treating Endometriosis. Obstet Gynecol. 2018 Aug; 132(2):475-477. PMID: 29995747.


Sperm morphology from the actual inseminated sample does not predict clinical pregnancy following intrauterine insemination – Dr. Jamie Stanhiser
Objective: To determine the effect of sperm morphology from the specific sample used for intrauterine insemination (IUI) on clinical pregnancy rates (CPR).
Design: Prospective cohort study.
Setting: Academic fertility clinic.
Patients: Couples undergoing IUI July 2016-January 2017.
Interventions: Morphology slides were prepared from the semen sample produced for IUI.
Main outcome measures: CPR was measured by detection of cardiac activity. Multiple logistic regression modeling was performed to determine the association of sperm morphology with CPR, controlling for age, antimüllerian hormone level, and post-wash total motile sperm count.
Results: Semen analyses, including Kruger strict criteria for morphology from the actual sample inseminated, were reviewed for 155 couples, comprising 234 total treatment cycles. The percent normal morphology significantly differed between the preliminary semen analysis and the IUI sample (-2.0% +3.7% (95% CI -2.55, -1.53). Of the total 234 treatment cycles, 8.6% resulted in clinical pregnancy. When categorized by strict morphology >4%, <4%, and <1%, the CPR was 6.6%, 9.8%, and 10.9%, respectively. In couples with otherwise normal semen parameters (isolated teratospermia), CPR by >4%, <4%, and <1% normal forms was 7.2%, 9.8%, and 11.1%, respectively. There was no significant association between the percent normal morphology and CPR in multivariate analysis.
Conclusions: This study evaluating the morphology of the actual inseminated sample did not find differences in CPR following IUI among couples with normal and abnormal sperm morphology, including severe teratospermia. Abnormal sperm morphology should not exclude couples from attempting IUI.
Stanhiser J, Mersereau J, Dock D, Boylan C, Caprell H, Coward RM, Berger DS, Fritz M. Sperm morphology from the actual inseminated sample does not predict clinical pregnancy following intrauterine insemination. F S Rep. 2020 Dec 9;2(1):16-21. PMID: 34223268.


Progesterone Receptor Status Predicts Response to Progestin Therapy in Endometriosis – Dr. Valerie Flores
Context: Progestin-based therapy is the first-line treatment for managing endometriosis-associated pain. However, response to progestins is currently variable and unpredictable. Predictive markers for response to progestin-based therapy would allow for a personalized approach to endometriosis treatment.
Objective: We hypothesize that progesterone receptor (PR) levels in endometriotic lesions determine response to progestin-based therapy.
Design: Retrospective cohort study.
Setting: Academic center.
Patients: Fifty-two subjects with histologically confirmed endometriosis and a previous documented response to hormonal therapy were included.
Interventions: Immunohistochemistry was performed on sections of endometriotic lesions using a rabbit polyclonal IgG for detection of PR-A/B.
Main outcome measures: The Histo (H)-score was used for quantifying PR status. Response to progestin-based therapies was determined from review of the electronic medical record.
Results: H-score was higher in responders compared with nonresponders. Subjects were categorized into three groups: high (H-score > 80, n = 7), medium (H-score 6 to 80, n = 28), and low (H-score ≤ 5, n = 17) PR status. The threshold of PR > 80 was associated with a 100% positive predictive value. The threshold of PR < 5 was associated with a 94% negative predictive value.
Conclusion: PR status is strongly associated with response to progestin-based therapy. Receptor status in endometriosis could be used to tailor hormonal-based regimens after surgery, and negate trialing progestin-based therapy to determine resistance. Ascertainment of PR status may allow for a novel, targeted, precision-based approach to treating endometriosis.
Flores VA, Vanhie A, Dang T, Taylor HS. Progesterone Receptor Status Predicts Response to Progestin Therapy in Endometriosis. J Clin Endocrinol Metab. 2018 Dec 1;103(12):4561-4568. PMID: 30357380.
Let’s Take the Next Step Together
Our skilled fertility specialists are here to help. Contact us today and let’s discuss the next phase of your fertility journey.
