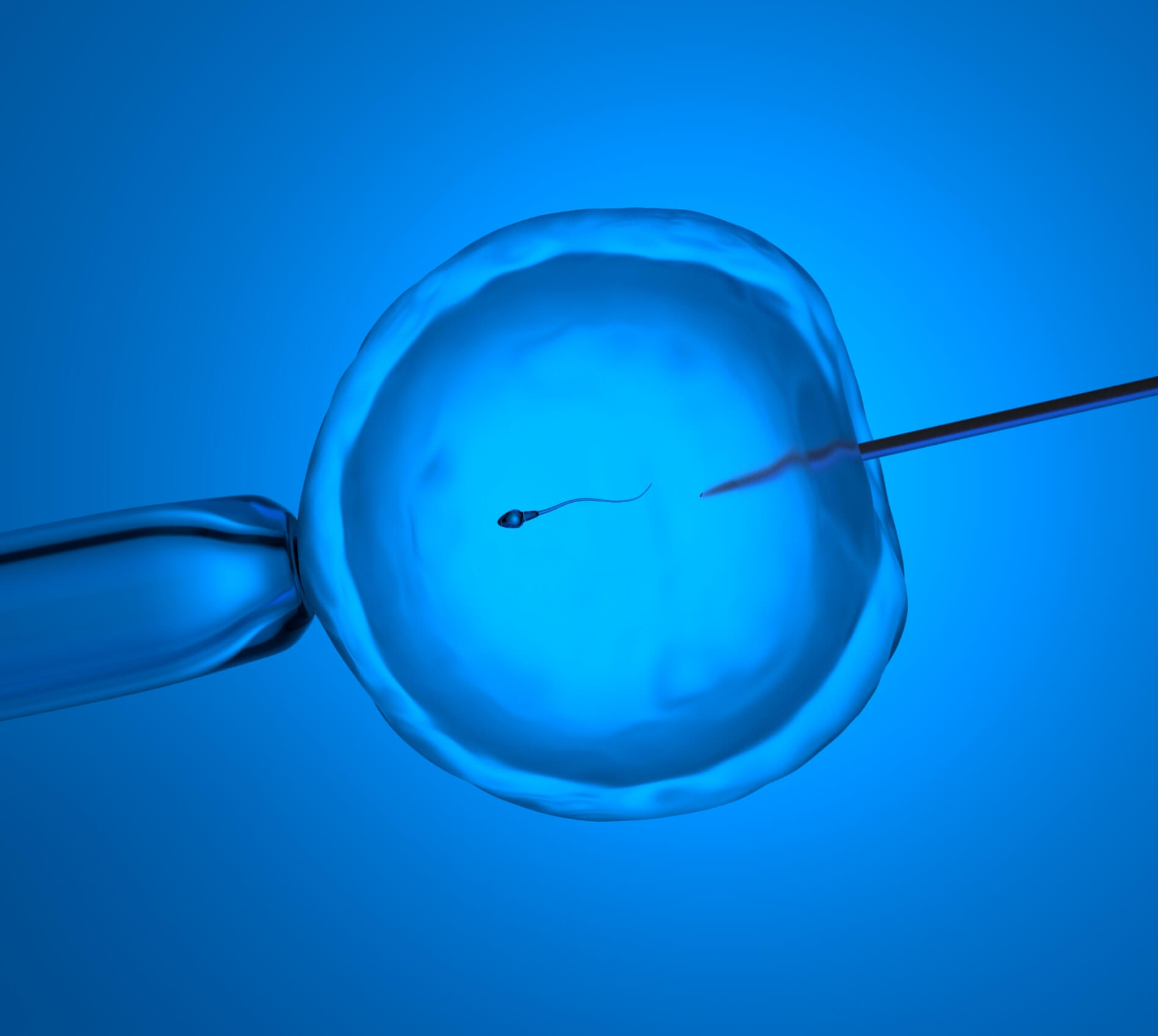
ICSI Process
The IVF cycle with ICSI is conducted similarly to a non-ICSI cycle, with a few exceptions. After the eggs are retrieved, instead of mixing the sperm with the egg, the embryologist uses a thin glass pipette to immobilize the sperm, draws it into the pipette and then injects it directly into the egg’s cytoplasm. Since the egg is the size of a pinpoint, it is a sophisticated technique requiring a high-powered microscope, tiny glass pipettes and instruments that translate hand movements into extremely fine movements of the pipettes.
The ICSI procedure has revolutionized the field of reproductive medicine, offering new hope for couples struggling with male factor infertility or previous failed IVF attempts. Our skilled embryologists are highly experienced in performing ICSI, ensuring the highest level of precision and success for our patients.

Let’s Take the Next Step Together
Our skilled fertility specialists are here to help. Contact us today and let’s discuss the next phase of your fertility journey.